Many of you have probably never heard of Cruetzfeldt-Jakob disease, but it is important to be aware of this severe and fatal degenerative neurological condition.
Although Cruetzfeldt-Jakob disease is rare worldwide, it is notably more common in Israel, particularly among those with Libyan ancestry.
Dr. Nurit Omar, director of the Huntington’s and Creutzfeldt-Jakob’s Disease Clinic at Sourasky Medical Center (Ichilov) in Tel Aviv explains how to recognize and deal with this disease.
First, it should be noted that this is an orphan disease, and that comes with consequences.
“Rare diseases [such as Cruetzfeldt-Jakob disease] are considered orphan diseases – diseases that are of less interest for researchers and pharmaceutical companies. That is very evident in this case,” Omar explained, noting that Cruetzfeldt-Jakob disease has a certain unique quality that has piqued research interest.
That uniqueness has to do with the protein in the body that causes it.
“[Cruetzfeldt-Jakob disease] is caused by a protein that acts like a virus or bacteria – it can infect other proteins. Until the 1960s, we thought it was just a virus. Then we realized the cause is a protein called a prion.”
Nurit Omar
“[Cruetzfeldt-Jakob disease] is caused by a protein that acts like a virus or bacteria – it can infect other proteins,” she explained.
“Until the 1960s, we thought it was just a virus. Then we realized the cause is a protein called a prion.”
A prion is a protein that has malformed, becoming abnormally folded. This change in its shape causes it to become “pathological and pathogenic – it wreaks havoc through the brain like a virus and infects other proteins, making them fold into prions. Then those proteins also become infectious.”
This process where prions infect normal proteins is very quick and is what causes Cruetzfeldt-Jakob disease to develop so rapidly.
“This neurodegenerative disease progresses faster than any other,” Omar said.
“Usually, from the moment symptoms appear, there is at most a year – usually less than that – before the patient dies.”
How is Creutzfeldt-Jakob disease diagnosed?
The symptoms of Cruetzfeldt-Jakob disease are varied. It can start with everything from behavioral changes, cognitive decline, difficulties walking and so on. All of these symptoms are by no means exclusive to Cruetzfeldt-Jakob disease and can be seen in other conditions. But what makes them stand out here is how rapidly the patient’s condition deteriorates.
“The disease progresses so quickly that more and more neurological deficits will manifest,” Omar said. “We know how to recognize Cruetzfeldt-Jakob disease because of how rapidly it develops.”
But aside from that, the other factor that helps spot the disease is a family history.
“This is a very rare disease worldwide, but it isn’t so rare in Israel. Here, the largest cluster of patients with the right genetics to develop this disease are those with Libyan and Tunisian ancestry,” Omar said, referring to a genetic mutation that is coded to cause proteins to turn into prions.
“People who know this disease know it from the ‘mad cow’ epidemic – there was an outbreak in the 1990s among cattle that transferred into humans who ate them. Many people got sick and because of the disease’s severity, they all died,” Omar said.
“This was also a prion disease and was a subtype of Cruetzfeldt-Jakob disease, though it probably doesn’t exist anymore. In Israel, we nearly only see the genetic type, related to hereditary mutation and not at all to eating meat.”
Even in Israel, though, the disease is still relatively rare. Even though there are many Israelis with Libyan ancestry, only a minority actually carry the mutation.
“There are around 200 families who carry this mutation and we see several dozen cases per year,” Omar said.
Most carriers will get sick and die, but there is hope on the horizon
How do you deal with a terminal disease without a cure or treatment?
According to Omar, there is still a lot that can be done.
“You can provide comfort and you can ease the suffering of both the patient and their family, for whom the suffering may be much worse,” she said. “Not only is a loved one sick with a terminal disease, but they realize they have a 50% chance of getting sick too.”
She added that the vast majority of carriers will show symptoms at some point, noting that it is a dominant inherited genetic mutation.
But even though there is no way to stop Cruetzfeldt-Jakob disease now, Omar stressed that “there is hope on the horizon.”
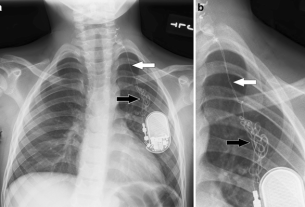
First, she said, Ichilov has a new test to check for the prions in spinal fluid. So far, these tests have a 100% success rate.
Second, every person who has a family history of Cruetzfeldt-Jakob disease has the right to undergo genetic counseling. This will help them learn the different possibilities and risks of having a child that doesn’t carry this genetic mutation.
In addition, there is also new and promising research in the field.
“The reason Cruetzfeldt-Jakob disease is of such interest to researchers today is that it is theorized that all, or at least most, degenerative disease function similarly to prion diseases,” Omar said.
“There are already several drug treatments for Cruetzfeldt-Jakob disease in development and one drug in particular that’s already in advanced stages and is expected to undergo clinical trials in humans sometime soon.”
This drug aims to change the genetic expression of the prion protein in carriers, which could hopefully prevent symptoms from manifesting.
“We are actively preparing for a cure and we have a large study in Ichilov with the family members of Cruetzfeldt-Jakob disease patients as participants,” Omar said.
“We gathered these relatives to try and understand the early signs that signal the earliest developments of the disease and to know the right time to start administering treatment.”