Israeli Breakthrough in the battle against deadly brain cancer
Researchers at Tel Aviv University activating the brain’s immune system against the deadliest cancer
Groundbreaking research from Tel Aviv University may lead to a significant breakthrough in the battle against deadly brain cancer.
The findings published in the leading scientific journal Nature Communications.
“Glioblastoma is the deadliest type of cancer in the central nervous system, accounting for most malignant brain tumors. It is aggressive, invasive, and fast-growing, making it resistant to existing treatments, with patients dying within a year of cancer’s onset.
Moreover, Glioblastoma is defined as a ‘cold tumor’, which means that it does not respond to immunotherapeutic attempts to activate the immune system against it.
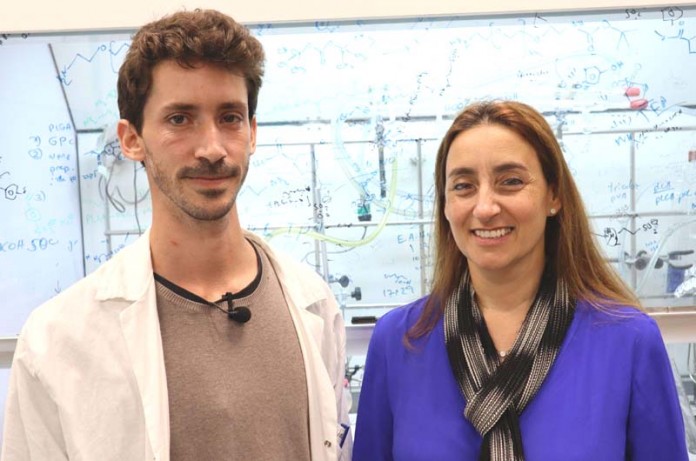
The Tel Aviv University researchers wanted to understand why the brain’s immune system (called microglia) does not inhibit the cancer. Led by Ph.D. student Eilam Yeini, they compared healthy brain tissues with glioblastoma tissues.
First, they identified a failure in the brain’s immune system in Glioblastoma cancer, leading to cell division and cell spread amplification.
The failure is caused partially by the secretion of a protein called P-Selectin (SELP). When bound to its receptor on the brain immune cells, it alters their function. Instead of inhibiting the spread of cancer cells, they do the opposite, enabling them to increase and penetrate brain tissues.
Next, the researchers were able to inhibit the secretion of the SELP protein, thereby neutralizing the immune system’s failure, restoring its regular activity, and blocking the spread of this incurable cancer.
“We wanted to understand why the brain’s immune system doesn’t do its job,” says Prof. Satchi-Fainaro, who won the Youdim, Bruno, Humboldt and Kadar Family Awards for Outstanding Research in 2020.
“We examined the interactions between the immune cells in the brain and the Glioblastoma cells in tumors that were recently removed from patients’ brains. To our surprise, we found that not only do the microglia cells do nothing to stop the cancer cells, they actually play a crucial and negative role by accelerating the division, spread and mobilization of glioblastoma cells.”
Since cells communicate with each other through proteins, the researchers checked what proteins are secreted when the microglia immune cells encounter the Glioblastoma cells, finding six overexpressed proteins. At the next stage, Prof. Satchi-Fainaro and her team blocked each of the six proteins, in turn, seeking to identify and isolate the one that enables the cancer to harness the brain’s immune system to its ends. Ultimately, they discovered that a protein called SELP is responsible for disrupting the immune system’s functions and boosting Glioblastoma tumors.
“SELP is a known protein that normally helps cells travel inside the body – especially white blood cells and endothelial cells that line the interior of blood vessels,” explains Prof. Satchi-Fainaro. “The encounter between Glioblastoma cells and microglia cells causes them to express SELP in large quantities. In the study, we were able to show that the overexpressed SELP helps the cancer cells travel and penetrate the brain tissue.”
After inhibiting SELP in pre-clinical Glioblastoma models, the researchers found that the tumor cells had a slower division rate, stopped migrating, and were less invasive. These results showed in animal models and 3D cancer models.
Dr. Asaf Madi’s laboratory at the Department of Pathology showed a decrease in the cancer cells’ malignant properties in a single-cell RNA sequencing.
He also points out that the immune system activation against the tumor SELP was silenced, and the communication between the microglia and Glioblastoma was disrupted. As a result, cancer’s progression in the brain was hindered.
The international research team was led by Prof. Ronit Satchi-Fainaro, Director of the Cancer Biology Research Center and the Head of the Cancer Research and Nanomedicine Laboratory at Tel Aviv University.
TAU researchers collaborated with neurosurgeons from the Tel Aviv Sourasky Medical Center (Ichilov) who supplied Glioblastoma tissue samples removed during surgery and also with neurosurgeons from Johns Hopkins University and the Lieber Institute in the USA, who supplied healthy brain tissues from autopsies.
Read more about: brain cancer, Tel Aviv University (TAU)