The Technion – Israel Institute of Technology and Sheba Medical Center have developed a cost-effective method for fabricating custom-made functional cosmetic implants for the rehabilitation of congenitally malformed ears.
Microtia is a birth defect condition in which the external ear does not grow normally, resulting in a small and irregularly shaped ear. Microtia occurs in between 0.1% and 0.3% of births. Occasionally, in addition to the visual concern, microtia results in hearing loss.
“Bones” of the outer ear – the auricle – are flexible cartilage rather than bone tissue. The standard procedure for microtia repair is to harvest costal cartilage from the patient’s chest. This procedure is painful, discomfort, and put the patient in risk of further complications. Additionally, building one ear that is identical to the other requires both inventiveness and advanced surgical abilities on the part of the surgeon.
The journal Biofabrication reported on the Israeli researchers’ breakthrough, which was made possible by a collaboration between Professor Shulamit Levenberg of the Technion’s Faculty of Biomedical Engineering and Dr. Shay Izhak Duvdevani, a senior physician in the Otorhinolaryngology-Head and Neck and head Surgery Department of the Sheba Medical Center’s Tissue Engineering Lab.
The current study used novel tissue engineering techniques established in Professor Shulamit Levenberg’s laboratory under the direction of Dr. Shira Landau at the Faculty of Biomedical Engineering at the Technion. They build a biodegradable auricle scaffold that created stable, custom-made neocartilage implants.
Dr. Shay Izhak Duvdevani, a senior physician in the Otorhinolaryngology Head and Neck Surgery Department and Head of the Tissue Engineering Lab at Sheba Medical Center participated in the research.
The one-of-a-kind scaffold, which enables the construction of an aesthetically pleasing and stable auricle, is 3D-printed and based on a CT scan.
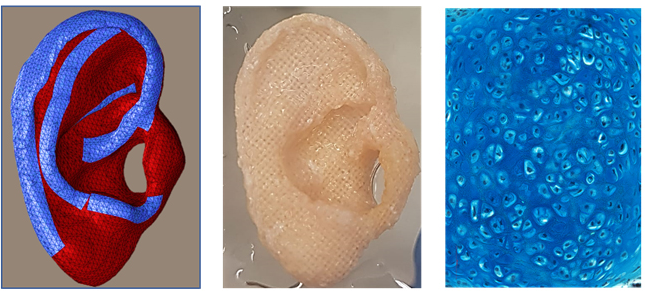
It is biodegradable and promotes the production of chondrocytes – the cells that produce cartilage – and mesenchymal stem cells. The scaffold contains pores of varying diameters, which facilitates cell attachment the formation to form solid cartilage.
According to the researchers, creating an auricle from a patient’s own cells will reduce the pain and risk associated with removing costal cartilage from children. Additionally, it will allow youngsters as young as six years old to undergo the procedure, rather than the existing common practice of waiting until they are ten. By doing the operation at an earlier age, the psychological impacts of microtia on children are likely to be mitigated.
The researchers observed cartilage growth within the auricle construct in the laboratory for 10 to 6 weeks before implanting it into a mouse. The outcome was satisfactory graft integration, and the prosthetic ear displayed excellent biomechanical function.
According to Prof. Levenberg, “One of the challenges in the study was to find a suitable 3D printing method, since fabricating an ear necessitates the use of biodegradable materials that break down in the body without harming it but have an extremely accurate external structure and small pores. We demonstrated all of this in the present research, and estimate that it will be possible to tailor our technology to other applications, such as nasal reconstruction and fabrication of various orthopedic implants.”
Dr. Duvdevani added that, “In the present study, we achieved a significant breakthrough by means of the integration of medicine and research and collaboration between doctors and researchers. This research is another milestone in the transition to advanced technologies in medicine, where the use of 3D printing and tissue engineering will play a significant part and provide patients with an optimal, state-of-the-art response.”