Immunotherapy matched to a specific patient to successfully treat patients using biological personalized medicine depends on suiting them to each other – but the technique is very complicated.
Now, researchers at the Ruth and Bruce Rappaport Faculty of Medicine and the Rappaport Family Institute for Research in the Medical Sciences at the Technion-Israel Institute of Technology have discovered a subset of blood cells that predict the success of immunotherapy treatment.
These findings are expected to streamline the process of matching an immunotherapy treatment to a specific patient since it is very important to identify in advance those patients who will react to a given treatment.
The study has just been published in the journal Cancer Cell under the title “Interferon-stimulated neutrophils as a predictor of immunotherapy response.” It was led by and contributed to equally by doctoral student Madeleine Benguigui and post-doctoral fellow Dr. Tim Cooper under the supervision of the faculty’s Prof. Yuval Shaked.
The translational research is based on RNA sequencing (scRNA-seq), analysis of existing data, pre-clinical models of cancer, and the corroboration of the findings in humans.
Immunotherapy, considered one of the most important breakthroughs in cancer treatment, is based on the understanding that the natural immune system excels at attacking cancer cells in a selective and precise manner.
The problem is that, in many cases, the cancerous tumor tricks the immune system and prevents it from identifying the cells as enemies. Immunotherapy is based on the concept that, instead of attacking cancer with chemotherapy drugs that also harm healthy tissue, it is preferable to boost the immune system with the goal of identifying cancer cells as enemies and letting it do the rest of the work on its own.
The effectiveness of the approach is still limited
Despite the remarkable success of the immunotherapy approach for treating cancer, its effectiveness is still limited to just 40% of all patients. This means that many patients receive this harsh treatment without positive results. As a result, it’s vital to have a deep understanding of biological reactions to these treatments and identify biomarkers that can predict the treatment’s future success.
Biomarkers are an important component of personalized medicine that helps doctors make educated medical decisions and formulate optimal treatment protocols adapted to the specific patient and their medical profile. They are already being used for immunotherapy treatments, but they are obtained through biopsies – an invasive procedure that can endanger the patient and be painful.
Moreover, this approach fails to sufficiently take into account the specific patient’s immune profile, and its predictive capability is limited. For this reason, a great deal of research in this field – both in industry and in academia – strives to find new ways to predict which patients will respond to immunotherapy treatments.
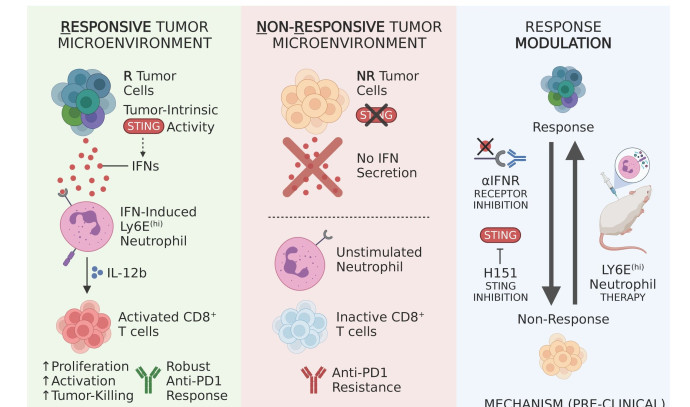
The researchers who focused on antibody-based immunotherapy discovered biomarkers that predict a specific patient’s response to the treatment. Since these are in the bloodstream, they don’t require taking biopsies. The team discovered that a protein called STING that activates the immune system is triggered by cancerous growths and is especially pronounced in cancer cells that will respond to immunotherapy treatment.
This protein is manifested in interferon protein, which in turn stimulates neutrophils to be differentiated into a specific type that expresses the protein Ly6Ehi) that acts directly on the immune system and stimulates it to target the cancerous tumor. Indeed, the researchers discovered that these neutrophils may help the actual treatment, as their presence in the tumor prompts greater sensitivity to immunotherapy treatment.
The researchers inferred that testing the levels of Ly6Ehi neutrophils in the patient’s blood could serve as an efficient biomarker for predicting the response to immunotherapy treatment. The researchers tested these findings, which were based on pre-clinical studies, on patients with lung cancer and melanoma.
These findings are consistent with the analysis of existing data on 1,237 cancer patients who underwent antibody-based immunotherapy treatments. Therefore, they demonstrated the neutrophils’ ability to predict, with a high degree of precision, response to immunotherapy in humans.
The technology of Shaked’s research group was registered as a patent and is in the midst of a tech-transfer process with the company OncoHost to continue its development. Shaked said that the technology can be used with the ubiquitous flow cytometry device that can be found in almost every hospital and is approved by regulatory agencies.
Various research groups from Israel and around the world took part in the research, including physicians and researchers from the Hadassah-University Medical Center, Rambam Health Care Campus, Sheba Medical Center, the University of Haifa, Heidelberg University, and Yale University.