A study done at Haifa’s Technion-Israel Institute of Technology shows that cell typing based on the expression of metabolic genes makes it possible to predict the patient’s response to immunotherapy. The researchers created a tool to predict which patients will respond to this therapy based on this therapy that shows the importance of metabolism in the tumor microenvironment.
Professor Keren Yizhak and Ofir Shorer from Rappaport Faculty of Medicine at the Technion-Israel Institute of Technology in Haifa have developed a new tool for this type of assessment based on the metabolism of immune cells in the tumor microenvironment. They have just published their findings in the journal iScience under the title “Metabolic predictors of response to immune checkpoint blockade therapy.”
While there have been efforts to determine in advance whether or not the drugs will be effective for specific patients, current tools for doing so – for example, based on a genetic signature or the number of different cells, are not accurate.
Since cancer cells and the immune system cells are found in the same environment, they are fighting over the same resources. Quantifying their metabolic demands enables successful prediction of the effect of ICI drugs on the individual patient. To accomplish that, they analyzed single-cell RNA-sequencing of 1,700 metabolic genes taken from more than one million immune cells of cancer patients treated with ICI.
A groundbreaking discovery
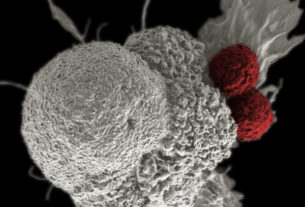
The introduction of immune checkpoint inhibitors (ICI) anti-cancer drugs is one of the most important revolutions in cancer medicine. These drugs are designed to deactivate a natural immune mechanism that can endanger patients who have a cancerous tumor. The immune mechanism in question is a network of “immune checkpoints.” Its role as a mechanism that regulates the immune system under normal conditions is to prevent the immune system from reacting with excessive force that could damage healthy cells.
But when faced with a cancerous tumor, that same mechanism can prevent the immune system from attacking the cancer cells. This is the background against which ICI drugs were developed; these drugs deactivate this mechanism and “free” the immune system to attack the cancer cells.
These drugs have caused a revolution in cancer medicine, leading to the inhibition of tumor growth in many kinds of cancer, but, unfortunately, these drugs are effective in fewer than 40% of patients. The rest of the patients suffer from side effects of the drug without enjoying any benefit.